Florida and Michigan dietitians this blog is for you
Florida and Michigan dietitians this blog is for you.
I get tons of questions from Florida and Michigan dietitians relative to credentialing and accepting insurance. Therefore, I thought it would be helpful to let you know what I know.
Let's start with Michigan
To the best of my knowledge, your state’s largest product Blue Cross Blue Shield of Michigan doesn’t allow Registered Dietitians to bill for MNT. This has to do with your lack of licensure. The BCBS Michigan product only allows licensed professionals to participate. So without a license, they don’t allow any dietitians to participate.
Your affiliate for Michigan has been working hard on changing this. And I am optimistic for change. But currently, you are unable to credential and bill Blue Cross Blue Shield of Michigan.
The same holds true for out-of-state providers for Blue Cross Blue Shield. If you are a provider who has a patient who has Blue Cross Blue Shield of Michigan when you call to verify their benefits the representatives will tell you the patient often has 6 covered MNT visits. This is a misquote of benefits. While they may quote you 6 covered visits, they will deny all 6 visits. For some reason on the BCBS of Michigan plans ONLY RDs can bill for MNT. Which makes no sense. BUT seems to hold true on these contracts.
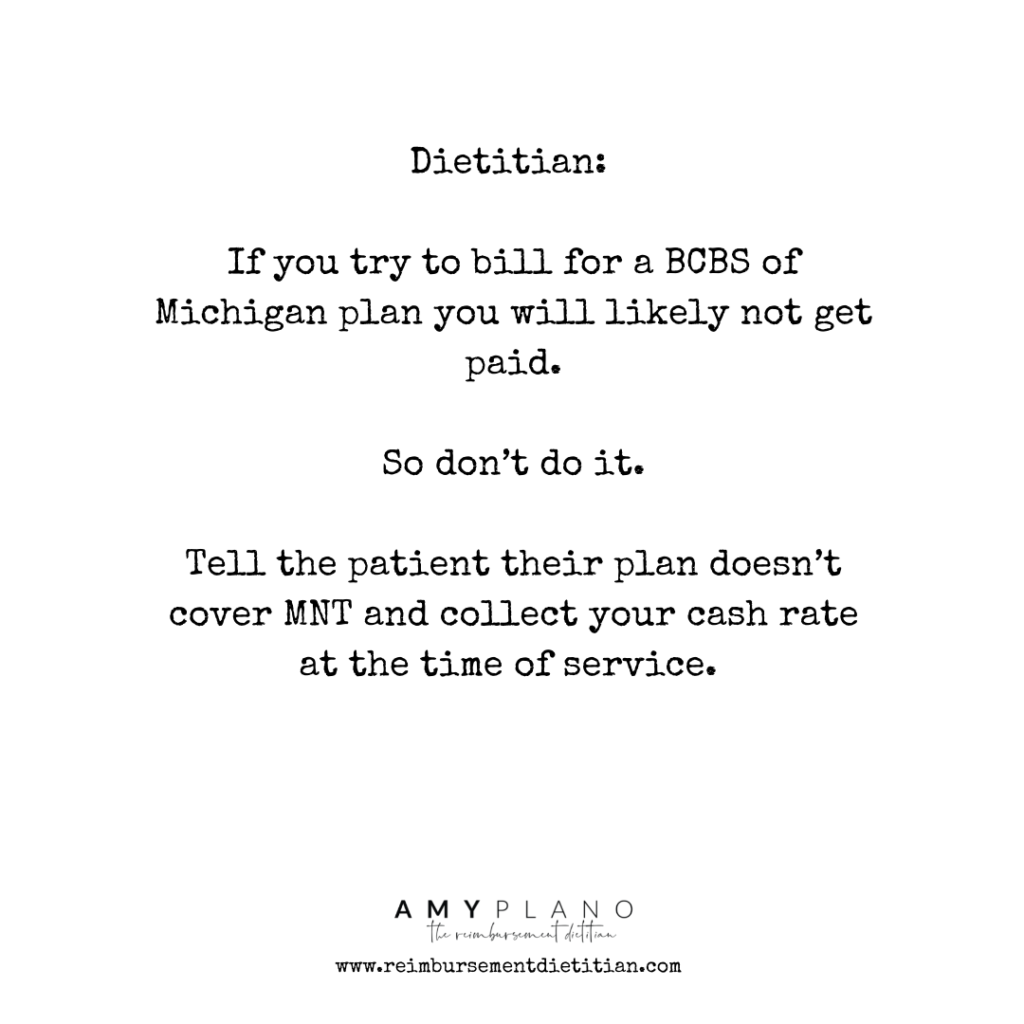
Therefore, if you try to bill for a BCBS of Michigan plan you will likely not get paid. So don’t do it. Tell the patient their plan doesn’t cover MNT and collect your cash rate at the time of service.
For whatever reason, the other national plans Aetna, Cigna, and United Health Care are also wonky. Some do accept Michigan-based providers. However, it is somewhat of a crapshoot In most areas in Michigan, as to whether or not you can participate and bill these products. I always say give it a shot – and request network status. The worst they can tell you is no.
On the positive side, Medicare (a federal plan) is open to Michigan dietitians to participate as providers. All Medicare products reimburse for MNT for patients with diabetes and chronic kidney disease stages 3a-5 (non-dialysis). As I will mention below, many of the Medicare plans are Advantage plans. These plans will require in-network participation with both Medicare and the commercial side of the plan.
The 411 for Michigan dietitians ...
In summary, due to your licensure limitations, your biggest insurance payer (BlueCross BlueShield of Michigan) will not allow dietitians to bill for MNT. This is not ALWAYS the case for the other national products (Aetna, Cigna & United Health Care). Often you can credential and bill for patients with these plans that have MNT coverage on their policies. However, call to see if this is an option for your practice. Medicare is also an option for dietitians in Michigan.
Now on to Florida ...
Now let’s chat about Florida and insurance.
Florida is a licensure state.
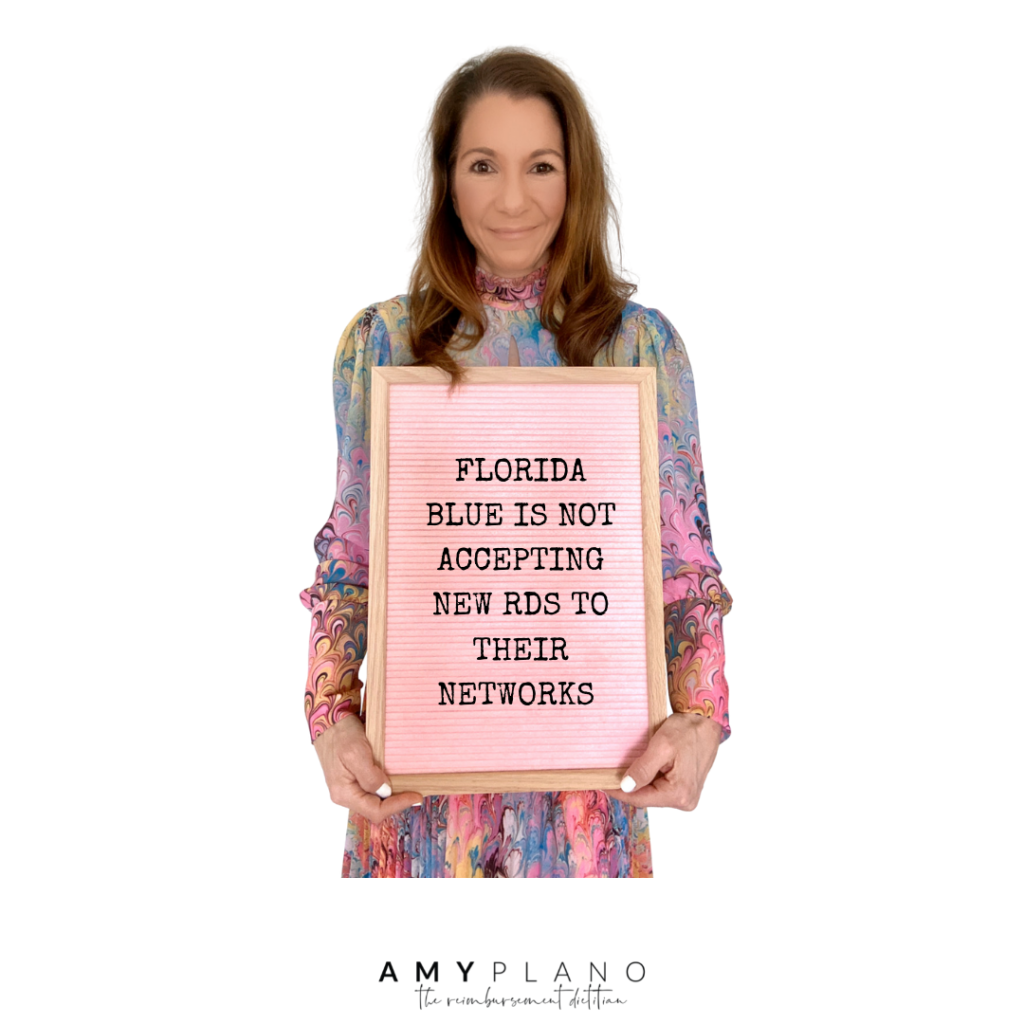
So while Florida-based dietitians don’t face issues related to licensure, they like Michigan experience issues with credentialing and billing their state’s BlueCross BlueShield product – Florida Blue.
Florida Blue insurance is not currently accepting any dietitians into their network. The way I understand this is twofold. One they are saying the ‘network’ is closed and is at capacity for dietitians. But on the other side, if you look at their network they don’t list ANY dietitians who actually participate.
On the flip side, if Florida Blue doesn’t credential dietitians then I think it’s fair to assume the majority of the policies will not cover MNT. So if you are an out-of-state dietitian credentialed with your home state plan, and you have a patient who has Florida Blue there is a good chance the patient doesn’t have MNT on their Florida Blue Policy. Some plans DO. But many plans don’t.
So proceed with caution when you bill for these patients.
In my experience, the commercial insurance plans at the time of me writing this post, Humana, and the Oscar networks are open to accepting new providers based in Florida. While this is in fact a positive for sure, these insurance companies are not super common payers in Florida.
Cigna appears to occasionally appear open to accepting new providers. It seems to be based on your zip code. While the Aetna and UnitedHealthcare networks are repeatedly closed due to the networks being at maximum capacity for dietitians.
It seems like the only way to credential with Aetna and UnitedHealthCare is if you are joining an existing group practice that has a pre-existing contract with these two insurance companies.
So my personal take on Michigan and Florida from an insurance standpoint?
I am very hopeful for Michigan dietitians. Given all the hard work the dietitians are putting into trying to make licensure a sure thing in Michigan, I feel in the future you will have access to Blue Cross Blue Shield of Michigan plans with MNT coverage. In the meantime, I would certainly credential with Aetna, Cigna, and United Health Care as well as Medicare if permissible. That way when something ‘gives’ with your BCBS product you will be ready to pounce on that opportunity.
Yes. BCBS is a sizable product. BUT given your potential access to join some of the other major networks that will diversify your insurance portfolio for your practice. Plus, in my experience, Aetna and UnitedHealthCare tend to be the most popular Medicare Advantage plans. So you should really be good to go with billing most Medicare plans.

Florida. I honestly don’t really understand the ‘why’ it is so difficult to work with the insurance companies in this state. Yes, your state has had some bumps in the road from a licensure standpoint. But currently, your license is not in jeopardy, and from what I know rock solid. I don’t know why Florida Blue doesn’t credential dietitians. Nor do I know why so few Florida Blue plans actually have MNT coverage. I can only tell you what I know.
Oscar, Humana, and Medicare are open for new providers to enroll. But like I mentioned the enrollment of these plans is not super high. Yes. You will get some patients. And yes these plans seem to offer decent coverage for MNT. But I personally don’t feel like this presents enough of an opportunity to go all-in with insurance.
Yes you can get into medicare but ...
While you can enroll and bill for Medicare. My main concern is most Medicare patients have Medicare Advantage Plans. These are Medicare plans managed through a commercial carrier like Aetna, Humana, Cigna, and United Health Care. The claims for the advantage plans typically (although not always) require you to be in with both Medicare and the commercial plan. These types of claims get submitted to the commercial payer. Therefore, I am concerned that given the major commercial networks are closed, you will even struggle with participating with Medicare at a level that makes sense.
So, that is all I got for you Michigan and Florida dietitians for now. Fingers crossed for a brighter future for the commercial networks in these states. I am rooting for you all.
Note: this point was posted on 4.15.22 just for a post a reference for the information posted in this blog.
