What CPT codes can dietitians use to bill?
Last week on the blog we chatted about what diagnosis codes (aka ICD-10 Codes) dietitians can bill with. This week I thought it would be fitting to discuss what CPT codes dietitians can use to bill. As you will see, these same CPT codes are applicable in any billing scenario: whether you are billing insurance directly or indirectly by providing the patient with an MNT Superbill.
CPT Codes Versus ICD-10 Codes
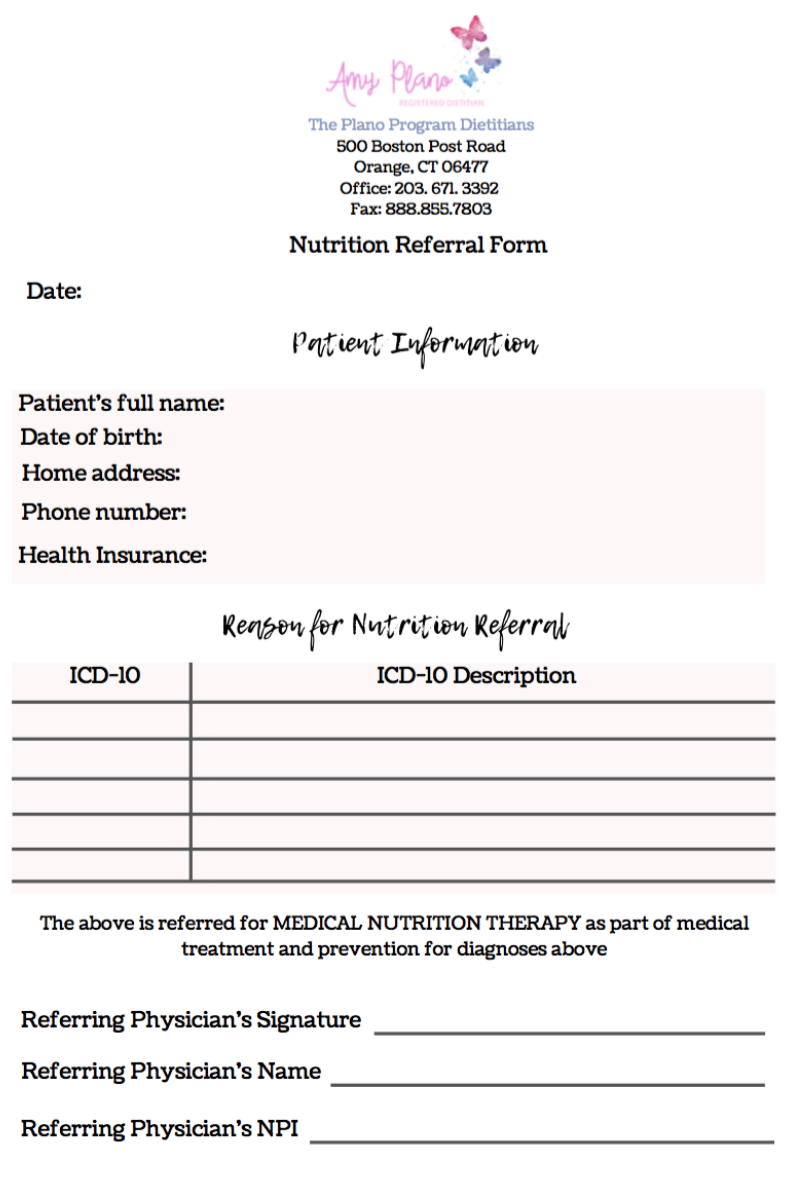
ICD 10 codes are different from the Current Procedural Terminology (CPT) codes. ICD-10 codes are used to describe a medical diagnosis. And like we discussed last week, it outside the scope of practice of a dietitian to make a medical diagnosis. Therefore, unless we are billing using preventative coding, then we always need to request a MNT referral for the patient we are going to be counseling with the correct ICD-10 code.
CPT codes are procedure codes that describe the service rendered by the healthcare professional. As you will see there are only a handful (3 to be exact!) of codes dietitians most commonly use. We don’t need a referral to determine which CPT code to use for the visit. We instead assign a CPT code to the visit based on the type of visit. In addition, we only use one CPT code per visit. While it it possible to use multiple ICD10 codes for a single visit. Furthermore, it is the CPT code determines the amount of reimbursement you will receive from a particular insurer not the ICD-10 code.
When you file a claim you will be using both ICD 10 code (s) and CPT codes.
CPT Codes Dietitians can use to Bill
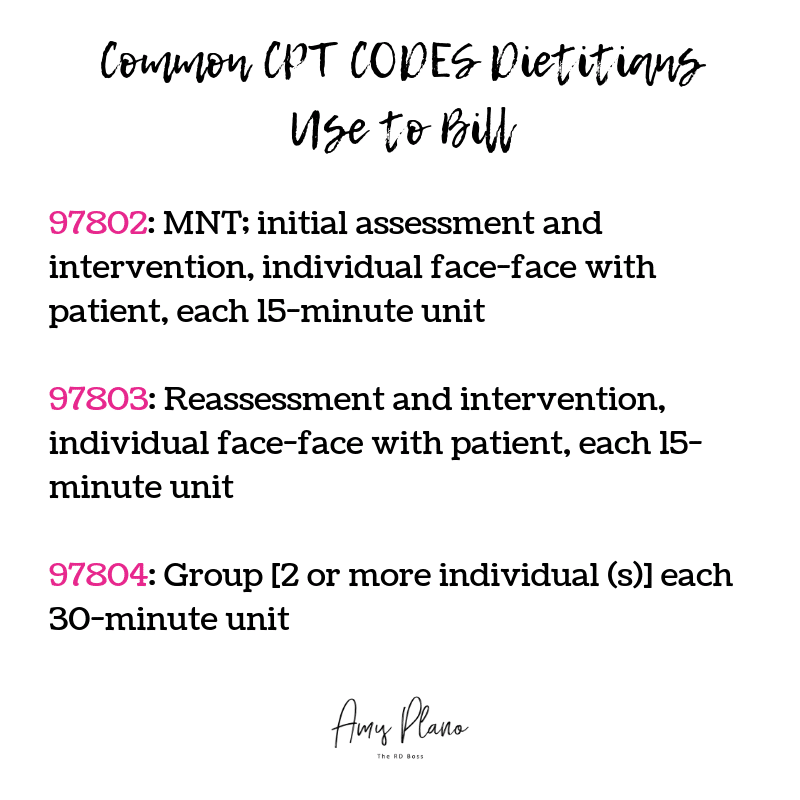
The Medical Nutrition Therapy (MNT) CPT codes dietitians can use to bill insurance companies are fairly standard. The most common CPT codes include:
Most health insurance companies accept the same three CPT codes 97802, 97803, and 97804. You will bill for the number of units you spend face-face with the patient using the corresponding CPT code.
- The difference between 97802 and 97803 is that you can only bill using CPT code 97802 once for an initial MNT patient visit with you. Please note that if your patient has seen a different dietitian and this is their first visit with you – then you can still use CPT code 97802. As this is the patient’s initial visit with YOU.
- You will use CPT code 97803 for all MNT nutrition visits beyond the initial visit.
- You will use CPT code 97804 to bill for MNT that you provide in a group setting involving 2 or more patients.
- In my experience, the highest payout value per unit is for the CPT code 97802 which you can only use once.
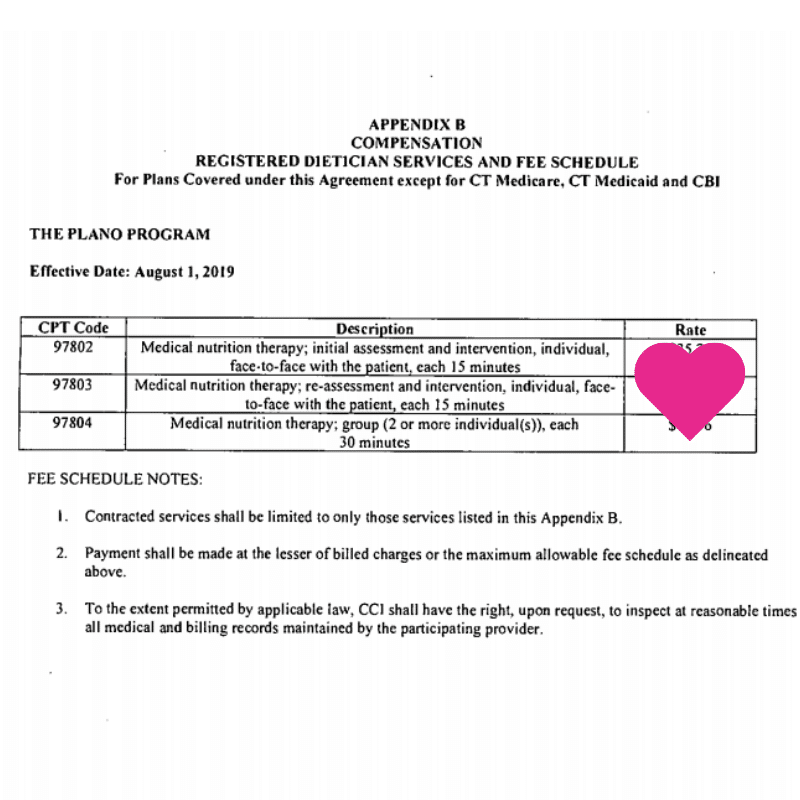
While there are certainly other CPT codes dietitians can use when billing health insurance, please note the CPT billing codes must be specifically listed in the dietitian’s insurer’s provider agreement/contract in order for an RDN to bill for it. Once you have gone through the credentialing process with each insurance company and are accepted, they will send you a contract. In the contract it will state the allowable CPT codes you can bill with. The contract will also describe the specific allowable compensation per unit billed. Therefore, while the CPT codes for most carriers are the same: 97802, 97803 and 97804 the compensation varies depending on the insurance company.
Here is an example of a recent contract I received for my group nutrition private practice: The Plano Program Dietitians.
While I can’t share the exact financial details of my particular contract, I use this sample to illustrate what a fee schedule will look like. It is typically located towards the end of your contract – often in the Appendix. As you can see, each of the CPT codes dietitians can use to bill is associated with a fixed rate. The rate does not change. Each time you bill a particular insurance company using 97802 you will receive the same compensation per 15-minute unit billed. The same goes for CPT codes 97803 and 97804.
Please keep in mind while your reimbursement rate is static for the course of your contract, whether or not the patient has coverage for these services is variable depending on their particular policy. Therefore, I would highly recommend having your patients verify their nutritional benefits PRIOR to their visit. Visit my personal private practice website to view the script I provide my patients for verifying their insurance benefits.
In addition, certain insurance companies allow for the use of Preventative Care CPT codes. I will dedicate an entire future blog on preventative coding for MNT in the future. It is a super exciting topic as it provides our patients with much more comprehensive nutrition counseling coverage.
Where on the insurance claim does the CPT code go?
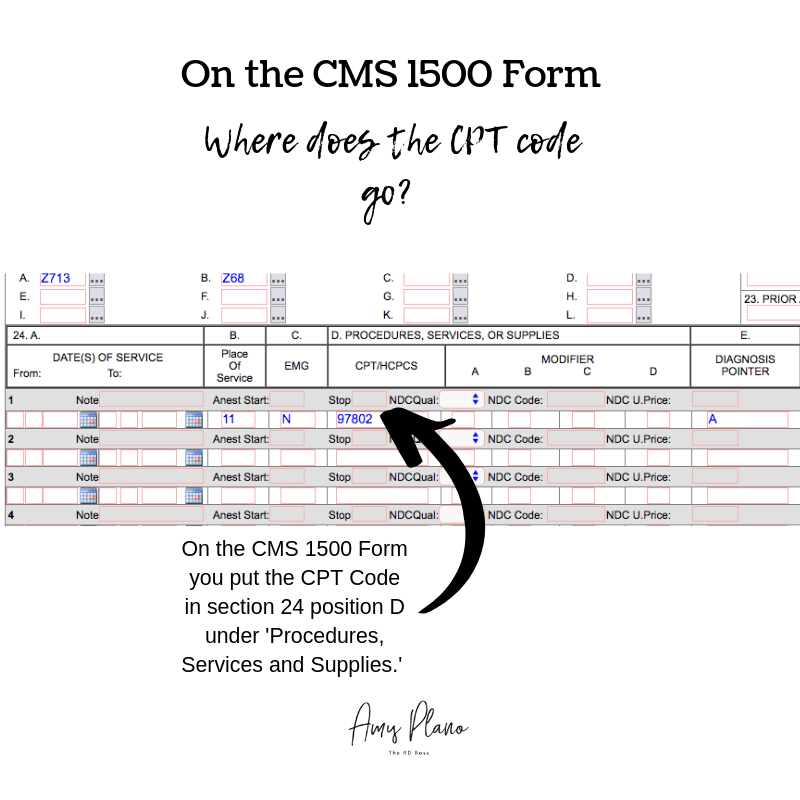
When billing a patient’s health insurance for MNT will always use a CMS 1500 form. For billing, I use the clearing house Office Ally. It used to be free. However, now many of the insurance companies I file claims for don’t participate with Office Ally, so I pay $70.00 per month to use the service. But in my mind, it is worth it as it allows me to bill electronically which saves me tons of time and aggravation.
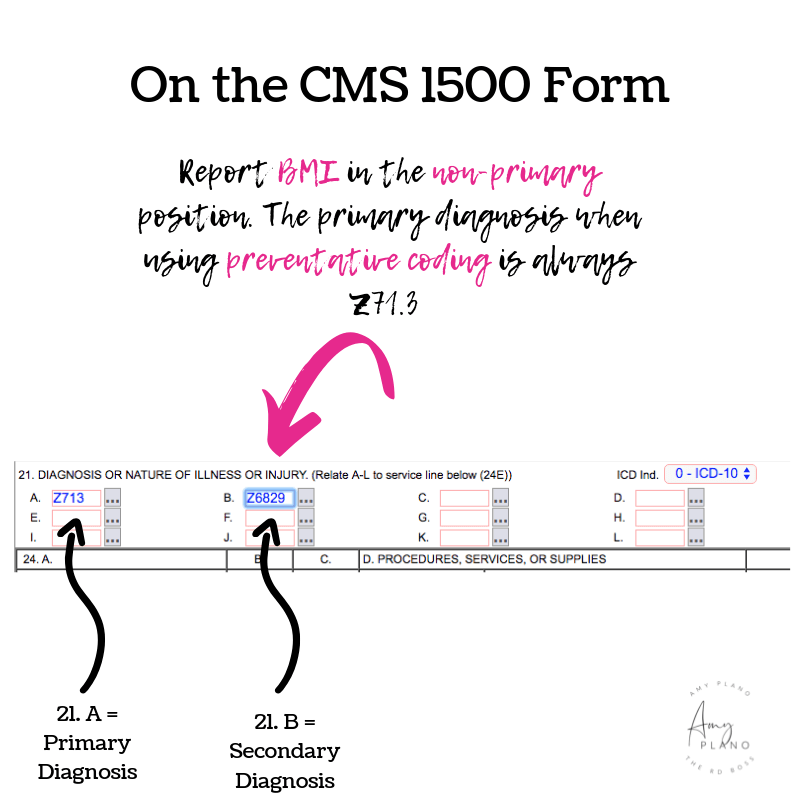
On the CMS 1500 Claim Form, you put the CPT code in section 24. location D. We refer to this section as the ‘Procedures, Services, or Supplies,’ area of the claim. The example in the image above represents a claim for an initial MNT assessment with the corresponding CPT code 97803. Luckily in Office Ally you can set up templates to use. For example, for each of the dietitians in my group, I have templates set up for an initial visit (97802) and a follow-up visit (97803). That way each time we bill for a patient we only need to click on the patient’s name, the type of visit and the date billed. Easy-peasy!
Need an MNT Superbill?
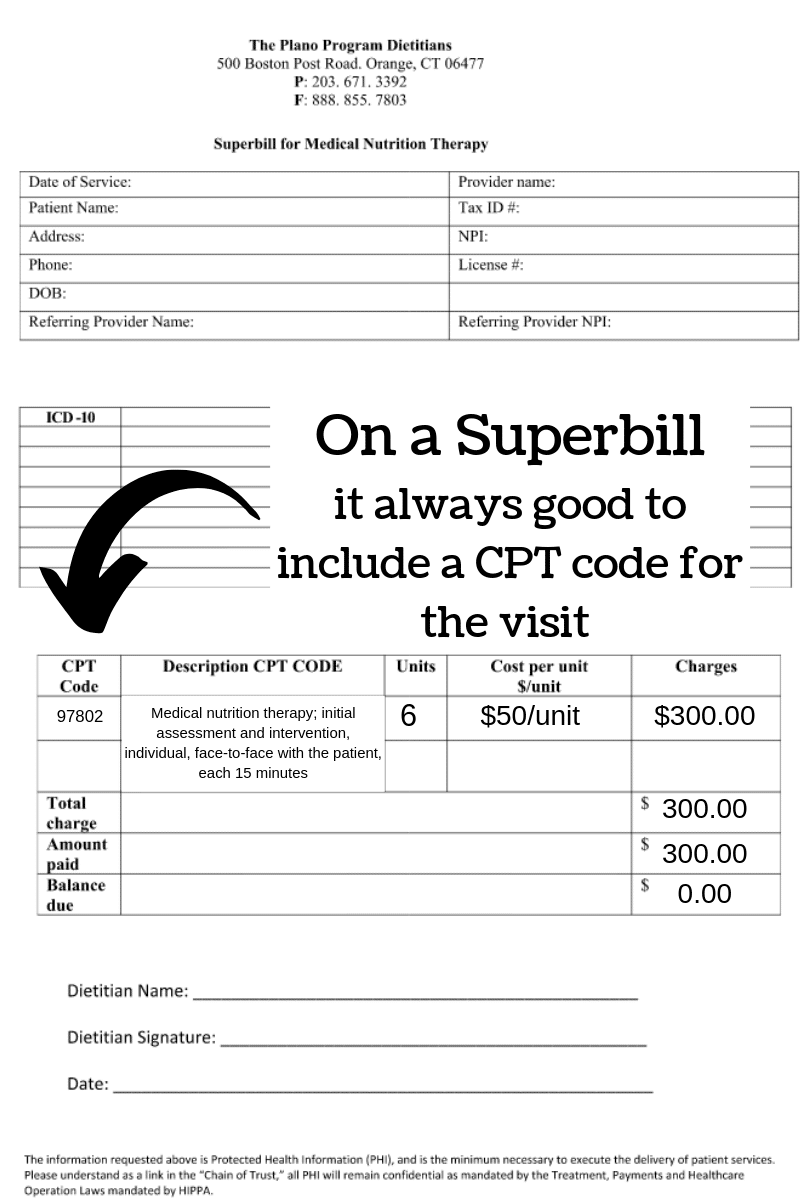
If you don’t yet have an MNT Superbill to use for your nutrition private practice please feel free to use the one I created for my practice. You can find it here located in the Resources section of The Reimbursement Dietitian’s website. I created it in Word so all you need to do is exchange your nutrition private practice’s information up top and you are good to go!
Where Should You Put the CPT Code on a MNT Superbill?
When should you provide an MNT Superbill to? You should provide an MNT Superbill to your patients whose insurance companies you don’t participate with. Or put another way – for insurance companies you are considered an out of network provider. The patient pays you first and THEN you provide the MNT Superbill. Think of a Superbill just like a receipt. The patient then submits the Superbill to their insurance company in an effort to collect reimbursement. The patient’s particular insurance policy will dictate whether or not they will be reimbursed for their visit. Below is an image depicting where you would place the CPT code for a patient’s visit on a MNT Superbill.
A Note about MNT Superbills
On the MNT Superbill I created you can easily edit the fields in Word. Depending upon the nature of the visit (initial or follow-up visit) you would write the appropriate CPT code and include a brief description of the CPT code. The units represent time blocks of 15 minutes. So, in the example above, 6 units would equal 90 minutes of face-face MNT counseling. When you are an out network provider insurance rates don’t apply to you. Therefore, you can use your personal established rates. Make sure to note the amount charged, the amount paid and whether or not there is a balance. A good rule of business with MNT Superbills is to collect all money up front – either charge the patient before their visit or no later than at the of service. That way you are not chasing your money!
Conclusion
Using the appropriate CPT code is critical to getting paid correctly and in a timely manner. The most common CPT codes dietitians can use to bill are : 97802, 97803 and 97804. The CPT codes 97802 and 97803 represent codes dietitians use to bill for individual MNT visits. While the CPT code 97804 would be used to bill for groups of patients of two or more. When billing insurance your particular contract will determine how much you are reimbursed for each unit billed. This value doesn’t change unless your contract changes. In future blogs I will discuss additional CPT codes dietitians can use to bill that are less common.
Need support in getting credentialed, growing your insurance-based practice, and making the money you deserve? Check out my coaching programs HERE. I teach dietitians how to get credentialed, bill the shit out of insurance and make some serious cheddar in their insurance-based practices.