What CPT codes can dietitians use to bill?
Last week on the blog we chatted about what diagnosis codes (aka ICD-10 Codes) dietitians can bill with. This week I thought it would be fitting to discuss what CPT codes dietitians can use to bill. As you will see, these same CPT codes are applicable in any billing scenario: whether you are billing insurance directly or indirectly by providing the patient with an MNT Superbill.
CPT Codes Versus ICD-10 Codes
ICD 10 codes are different from the Current Procedural Terminology (CPT) codes. ICD-10 codes are used to describe a medical diagnosis. And like we discussed last week, it outside the scope of practice of a dietitian to make a medical diagnosis. Therefore, unless we are billing using preventative coding, then we always need to request a MNT referral for the patient we are going to be counseling with the correct ICD-10 code.
CPT codes are procedure codes that describe the service rendered by the healthcare professional. As you will see there are only a handful (3 to be exact!) of codes dietitians most commonly use. We don’t need a referral to determine which CPT code to use for the visit. We instead assign a CPT code to the visit based on the type of visit. In addition, we only use one CPT code per visit. While it it possible to use multiple ICD10 codes for a single visit. Furthermore, it is the CPT code determines the amount of reimbursement you will receive from a particular insurer not the ICD-10 code.
When you file a claim you will be using both ICD 10 code (s) and CPT codes.
CPT Codes Dietitians can use to Bill
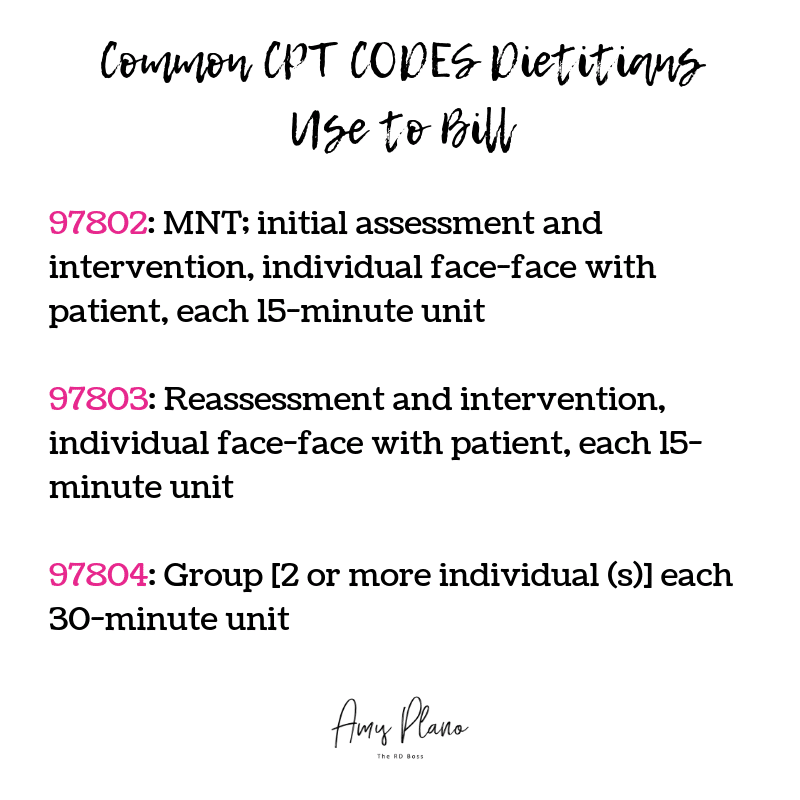
The Medical Nutrition Therapy (MNT) CPT codes dietitians can use to bill insurance companies are fairly standard. The most common CPT codes include:
Most health insurance companies accept the same three CPT codes 97802, 97803, and 97804. You will bill for the number of units you spend face-face with the patient using the corresponding CPT code.
- The difference between 97802 and 97803 is that you can only bill using CPT code 97802 once for an initial MNT patient visit with you. Please note that if your patient has seen a different dietitian and this is their first visit with you – then you can still use CPT code 97802. As this is the patient’s initial visit with YOU.
- You will use CPT code 97803 for all MNT nutrition visits beyond the initial visit.
- You will use CPT code 97804 to bill for MNT that you provide in a group setting involving 2 or more patients.
- In my experience, the highest payout value per unit is for the CPT code 97802 which you can only use once.
While there are certainly other CPT codes dietitians can use when billing health insurance, please note the CPT billing codes must be specifically listed in the dietitian’s insurer’s provider agreement/contract in order for an RDN to bill for it. Once you have gone through the credentialing process with each insurance company and are accepted, they will send you a contract. In the contract it will state the allowable CPT codes you can bill with. The contract will also describe the specific allowable compensation per unit billed. Therefore, while the CPT codes for most carriers are the same: 97802, 97803 and 97804 the compensation varies depending on the insurance company.
Here is an example of a recent contract I received for my group nutrition private practice: The Plano Program Dietitians.
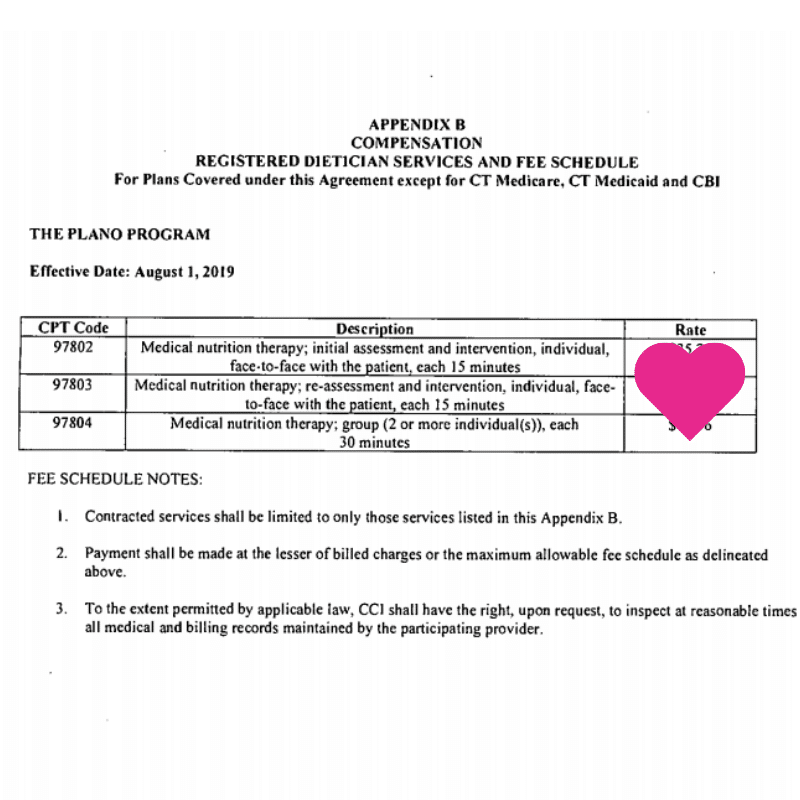
While I can’t share the exact financial details of my particular contract, I use this sample to illustrate what a fee schedule will look like. It is typically located towards the end of your contract – often in the Appendix. As you can see, each of the CPT codes dietitians can use to bill is associated with a fixed rate. The rate does not change. Each time you bill a particular insurance company using 97802 you will receive the same compensation per 15-minute unit billed. The same goes for CPT codes 97803 and 97804.
Please keep in mind while your reimbursement rate is static for the course of your contract, whether or not the patient has coverage for these services is variable depending on their particular policy. Therefore, I would highly recommend having your patients verify their nutritional benefits PRIOR to their visit. Visit my personal private practice website to view the script I provide my patients for verifying their insurance benefits.
In addition, certain insurance companies allow for the use of Preventative Care CPT codes. I will dedicate an entire future blog on preventative coding for MNT in the future. It is a super exciting topic as it provides our patients with much more comprehensive nutrition counseling coverage.
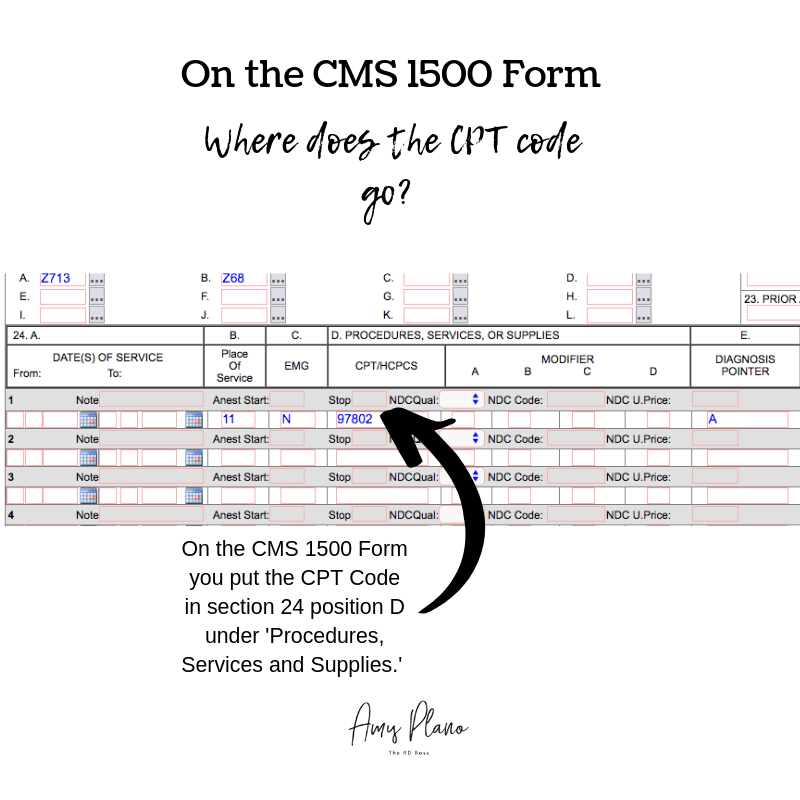
Where on the insurance claim does the CPT code go?
When billing a patient’s health insurance for MNT will always use a CMS 1500 form. For billing, I use the clearing house Office Ally. It used to be free. However, now many of the insurance companies I file claims for don’t participate with Office Ally, so I pay $70.00 per month to use the service. But in my mind, it is worth it as it allows me to bill electronically which saves me tons of time and aggravation.
On the CMS 1500 Claim Form, you put the CPT code in section 24. location D. We refer to this section as the ‘Procedures, Services, or Supplies,’ area of the claim. The example in the image above represents a claim for an initial MNT assessment with the corresponding CPT code 97803. Luckily in Office Ally you can set up templates to use. For example, for each of the dietitians in my group, I have templates set up for an initial visit (97802) and a follow-up visit (97803). That way each time we bill for a patient we only need to click on the patient’s name, the type of visit and the date billed. Easy-peasy!
Need an MNT Superbill?
If you don’t yet have an MNT Superbill to use for your nutrition private practice please feel free to use the one I created for my practice. You can find it here located in the Resources section of The Reimbursement Dietitian’s website. I created it in Word so all you need to do is exchange your nutrition private practice’s information up top and you are good to go!
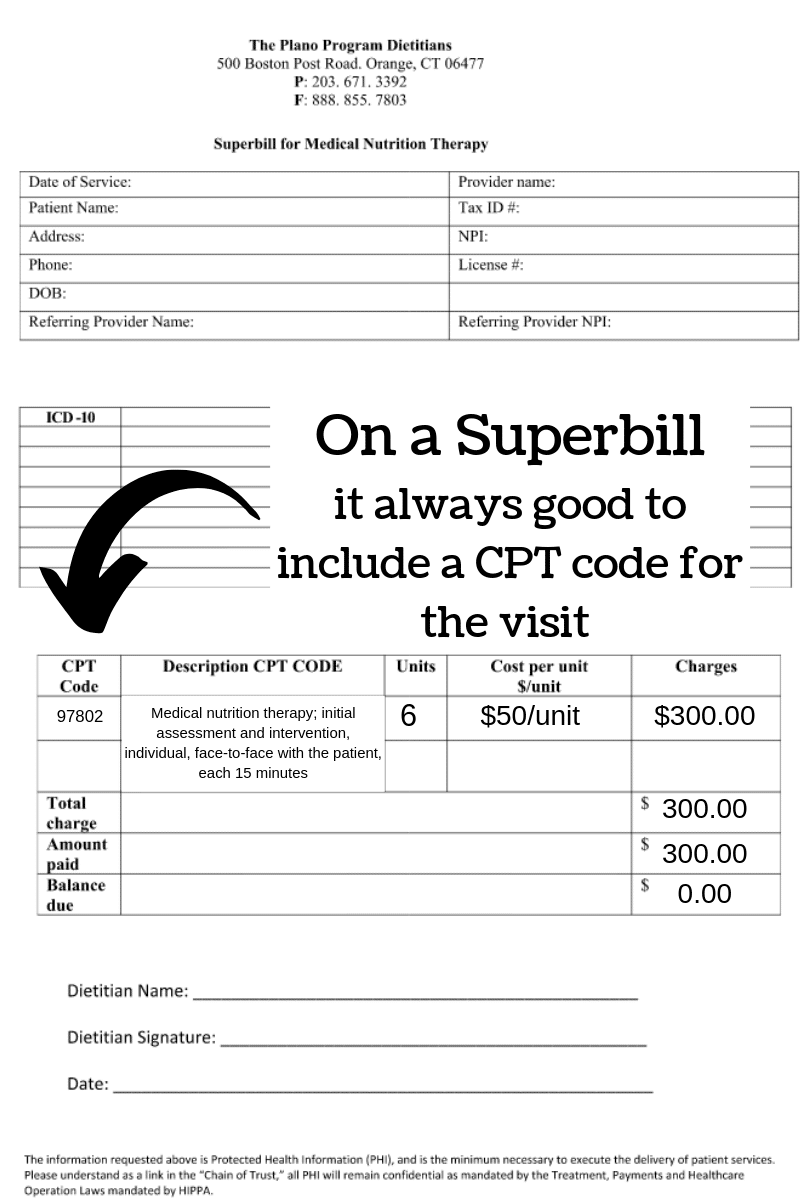
Where Should You Put the CPT Code on a MNT Superbill?
When should you provide an MNT Superbill to? You should provide an MNT Superbill to your patients whose insurance companies you don’t participate with. Or put another way – for insurance companies you are considered an out of network provider. The patient pays you first and THEN you provide the MNT Superbill. Think of a Superbill just like a receipt. The patient then submits the Superbill to their insurance company in an effort to collect reimbursement. The patient’s particular insurance policy will dictate whether or not they will be reimbursed for their visit. Below is an image depicting where you would place the CPT code for a patient’s visit on a MNT Superbill.
A Note about MNT Superbills
On the MNT Superbill I created you can easily edit the fields in Word. Depending upon the nature of the visit (initial or follow-up visit) you would write the appropriate CPT code and include a brief description of the CPT code. The units represent time blocks of 15 minutes. So, in the example above, 6 units would equal 90 minutes of face-face MNT counseling. When you are an out network provider insurance rates don’t apply to you. Therefore, you can use your personal established rates. Make sure to note the amount charged, the amount paid and whether or not there is a balance. A good rule of business with MNT Superbills is to collect all money up front – either charge the patient before their visit or no later than at the of service. That way you are not chasing your money!
Conclusion
Using the appropriate CPT code is critical to getting paid correctly and in a timely manner. The most common CPT codes dietitians can use to bill are : 97802, 97803 and 97804. The CPT codes 97802 and 97803 represent codes dietitians use to bill for individual MNT visits. While the CPT code 97804 would be used to bill for groups of patients of two or more. When billing insurance your particular contract will determine how much you are reimbursed for each unit billed. This value doesn’t change unless your contract changes. In future blogs I will discuss additional CPT codes dietitians can use to bill that are less common.
Need support in getting credentialed, growing your insurance-based practice, and making the money you deserve? Check out my coaching programs HERE. I teach dietitians how to get credentialed, bill the shit out of insurance and make some serious cheddar in their insurance-based practices.

Reader Interactions
Office Ally is $70 a month. I thought it would be less than a CRM like Healthie or Simple Practice!? Then may as well use those? I dont understand I shut off CRM to do billing on my own so I could save. I’m just starting and dont have many clients. Please advise thanks!
Hi Rolanda! It is $35 per user depending on the number of claims. So at the time, I wrote the blog I had one other RD. Now I have a team of three. I just switched to Simple Practice and for my group, it is around $140 per month. Simple Practice is the best if you are an RD primarily billing insurance. If you want a referral link for Simple Practice (it will save you $50 for your first month) please shoot me an email amy.plano@yahoo.com
I just became credentialed with MOHealthNet (Medicaid). And, I just found out in their fee schedule that these CPT codes are listed as Do Not Pay, meaning they aren’t covered. I am so disappointed. I found other CPT codes for telehealth only, which I do, and they are covered. Would trying to bill for those (I found 99421-99423 which is
“Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5–10 minutes”) be bad/wrong/illegal? I understand this is a complicated question- PS I love what you do!
Hi Amelia –
Unfortunately, MOST states have no MNT coverage for RDs in private practice for Medicaid. Therefore, even though you may be able to get credentialed due to the lack of coverage you can’t bill and expect to get reimbursed for the service. It is such a bummer and I am fighting hard in CT for this coverage as our patients desperately need our help. However, 99421-99423 aren’t within our scope of practice so you will not be able to bill for those codes. Typically we bill using 97802 & 97803. We can bill for groups (97804) as well. I am so sorry to hear about your CPT codes issues. Sending good karma your way for a successful insurance-based practice. Hugs & High Fives – Amy
Hello, we have had clients get denials when they switch insurance plans because the new plan does not have record of the initial session 97802 and thinks we are billing 97803 without it. These are a pain to fix through reconsideration. Do you know if it’s okay to bill 97802 as the first appointment on a new plan even if you’ve already been seeing the client? Or can you only bill 97802 once for the client ever?
Honestly – we only use 97802 for an initial visit or if we have not seen the patient in > 1 year. We never use when they switch insurances – as technically it is NOT an initial visit. I hope this makes sense!
If a patient only has Medicare A&B coverage and needs nutrient therapy how much does it cost for a face to face encounter and a telehealth phone visit. cpt code 97802.
Hi Lisa! I am not sure what you mean by nutrient therapy? Can you please clarify? MEdicare covers 100 percent of the cost for MNT – no copay no deductible.
As an RD, when working under a chiropractor in a chiropractic office setting, can we bill through their insurance or do we need to set up an individual reimbursement payment plan?
You will need to set up your own contracts – as RDs bill with different CPT codes and have a different scope of practice than chiropractors.
Hello! Can you tell me if there are different CPT codes for nutritional counseling versus medical nutrition therapy (MNT)?
Hi Cassandra – there are ONLY MNT codes. They are the same thing as nutritional counseling. There is NO difference. I hope this helps! Hugs & High Fives – Amy
Hello. How do bill for non-face to face time with client, meaning time spent for research and development of nutrition care plan? And, how much time is acceptable?
You CANNOT bill insurance for any time not with the patient not face:face providing MNT. If you find you need to do extensive research then you might need to bill the patient your hourly rate for those services.
Unfortunately that time is already factored into the CPT codes we bill with. That is why we are paid more for an initial visit than a follow up. More time is needed to develop the plan of care.
Hi Amy, The new RTM Codes under CMS for 2022 should allow additional reimbursement for time spent communicating with a patient even electronically. AMA must recognize these codes, although private insurers are not required to pay. Medicare and Medicaid do pay. These are not E/M codes.
Correct! But unfortunately, we have not seen any of the commercial plans allow us (or at least reimburse) these new codes. Also even for Medicare/Medicaid, there are stipulations to the best of my knowledge if and when the codes you are referring to can be used.
Hi. How many minutes are required to bill for 1 unit? For example, if you do a 28 minute appointment can you bill for 2 units? What’s the cut off? Thanks!
It is based on the rule of 8. Here is how you figure out the cut off values https://www.medicarefaq.com/faqs/medicare-8-minute-rule/
As a dietitian seeing a patient with another provider (MD, NP, SLP, etc) using a multi-disciplinary model, how does that change billing practice? Can the RD bill based on time and the other providers bill based off service?
All of our CPT codes are based on time. So you would just bill based on the amount of time you personally spent providing MNT to the client using the appropriate ICD 10 code and CPT code that represents the service.
When adding a test like a metabolic REEVUE test with CPT code 94690 that insurances remiburse for, do you add that as a “modifier”?
unfortunately, it is super rare for that code to get reimbursed by most commercial plans as it is outside of our scope of practice. I can’t imagine there would be a modifer as it is not telehealth or preventative service. We never bill insurance because the payout for RMR testing is quite low (<$75) or under. And we charge $150 for it in my practice - so it seems like a no-brainer for us.
In private practice I’ve been using the 02 location code for telehealth when working with clients from my office in their homes or work. On 4/1/22 CMS says location code 10 should be used for location in patient’s home. Can you clarify and is there more to this than I’m understanding?
Hi Maria – Each insurance company requires we bill using a different format for telehealth. Currently March 2022 there is no universal billing for telehealth. You need to check with each insurance company to confirm how they are requiring telehealth be indicated on the claim. Unfortunately each insurance company is different.
Is pre authorization required for using an aca wellness benefit? Using codes 97802 and Z71.3?
I am not sure – each POLICY is different! When you call to verify you will ask if reauthorization is required.
I am a credentialed RD with a handful of insurance companies, but still waiting on others.
Can we see patients and bill as incident to physician, for those patients that I am not credentialed with yet?
No – not unless you want the money to go to the MD. You will need to be credentialed to bill incident to them as well.
97802-97803 I understand as the office visit with a dietitian, but are there different codes for the actual meal plan and any supplements?
No – no CPT codes for those services. Those services CANNOT be billed to insurance. Check out my Master Classes on a la carte services https://the-reimbursement-dietitian.mykajabi.com/main-landing-page-for-reimbursement-master-classes-1 I explain this all in this class
I work as a virtual dietitian providing MNT services. I am considering offering group classes (covering topics such as nutrition fundamentals, diabetes prevention/management, nutrition & mental health, etc.) to my clients & other clients within my company. When I worked in an inpatient setting, I know the facility was able to bill insurance for group nutrition classes, but do you know anything regarding billing for this service virtually? Thanks!
Yes you can bill outpatient for group MNT classes. I teach how to do this in my reimbursement course
Would there be a CPT code we can use on a superbill for an online course that we create? My course is all delivered as pre-recorded videos (not live), and also includes live virtual group coaching sessions. They pay a lump sum for all of it. Also wondering if you know if HSA/FSA cards can be used for people to purchase our online courses or digital products?
Unfortunately, you can only bill insurance for MNT – so there is no CPT code for a course. Often HSAs can in fact we used for courses. However, they will also generally need an invoice to accompany them for the client to submit.
We have MNTs that want to do home visits for patients with ESRD etc what is the cpt code for a home visit for a nutrition therapy?
Unfortunately there is no CPT code that describes that service. You would need to reach out to the insurance company and get a specific place of service added to your contracts.
Hi Amy,
In this post you stated you would do another post about Preventative CPT codes. I am curious as to what these are, as many insurance companies are requiring the MNT to be “preventative” for there to be coverage. Do these codes help justify the insurance reimbursement for those patients?
Hi Kayla – my CheatSheet listed under my stores has the most current coding for all of the major insurance companies for preventative billing. You can find it here https://the-reimbursement-dietitian.mykajabi.com/cheat%20sheet%20for%20billing%20insurance
Thank you so much for your post! I was wondering if you had any insight on how to code for nutrition education and counseling during pregnancy and postpartum? Is there any way to get insurance to reimburse?
It will always depend on the plan and policy. Education by itself is never covered – but MNT pre/peri/post pregnancy would be. I teach what and how to code in my coaching programs. Each insurance company will allow fo different codes!
Hi Amy, do you know of a way to get around a patient’s deductible when billing for G0109 with a diagnosis of DM? Is there a limit typically to 97804 with a preventative code? Thanks so much!
No – if a Medicare patient has a deductible that isn’t satisfied and doesn’t have a supplement there is no way around it. Yes. 97804 is bound to the same exact restrictions on a patient’s plan as 97802/03 – you will always need to verify to determine the total allowable visits per service code
PHE during Covid allowed us to bill for MNT using hcpcs 97802 and 97803 but PHE is ending on 5/11/2023. However, I believe they are allowing an extension of MNT telehealth services beyond this date. Is that true?
Those ‘rules’ are only relative to Medicare which is a federal insurance company. Each state and insurance plan has its own rules regarding telehealth – in most states it is still active and there are no issues with telehealth. You need to check with the telehealth guidelines for each plan (how they want billed) as well as your state’s rules —
Hi Amy, have you ever billed cpt 99404 for follow up appointments for RD using preventive codes?
Yes we use those codes for in person visits for Cigna
Yes we use those codes for in-person visits for Cigna
New to private practice and billing. What Institutional Bill Type would I put in when submitting a charge for services rendered in a private setting not affiliated with a hospital/medical center.
Thank you,
Amy
All the codes noted here are used in a private practice setting —
Hi! I would with pediatrics and have multiple insurance contracts. I have not been able to get any appts reimbursed. I use 97802 and 97803. Do you have any suggestions for ICD 9 codes to bill? I have not been able to collect for any of them despite being told their insurance covers nutrition. if not, do have any suggestions or resources I can investigate. I have actually stopped taking clients because the families want to use insurance.
Ok! I think you mean ICD 10 codes (not 9) If you use ICD 9 code the claims will get denied. It will depend on the patient plan and policy – most plans DO cover pediatrics – an many accept Z71.3 + pedi BMI codes.
When billing insurances using Code 97802, 97803,97804 in the Description it states for each 15 min. If it is an initial consult and seen face to face. do will bill the code with a modifier for 4 units?
If the visit is in person then you bill with POS 11 — if it is telehealth you follow what ever is required for each insurance company to identify telehealth. 97804 is billed in units where 1 unit = 30 minutes
1-Is there usually a limit on the number of units you can bill for 97804. I know each plan will vary and we would need to ask but generally speaking do they limit to 1 unit or pay out 2 units (60min) or more?
2-In groups more than 2 have you ever seen this done virtually or large groups like for MNT nutrition education. Example if you had a MNT session that was 20 online virtual patients as part of a group nutrition course?
Yes – in my experience most plans allow for 2 units per DOS. YES! we have done a ton of large virtual MNT for big groups.