There seems to be a significant amount of confusion among dietitians and diagnosis codes. Hey yo! The Reimbursement Dietitian is here to tell you IT IS NOT WITHIN THE SCOPE OF PRACTICE OF A DIETITIAN TO MAKE A MEDICAL DIAGNOSIS. Therefore, I thought it would be super helpful in this blog to discuss three important aspects of billing with you: 1) what is a diagnosis code 2) what diagnosis code(s) dietitians can use and 3) how to obtain a diagnosis code.
So, let’s get to it!
What the heck are diagnosis codes?
Diagnosis codes are also known as ICD-10 codes. They are formerly referred to as the International Classification of Diseases (ICD), 10th Revision, Clinical Modification. These codes describe an individual’s disease or medical condition. Physicians determine the patient’s diagnosis and chart this in their medical records.
Need a good laugh? Read The Reimbursement Dietitian resource on “Is nutrition Private Practice Right for you? ” to learn about the time I mistakenly billed thousands of dollars worth of claims using the old ICD-9 codes. Tears and lots of headaches my friends. Lots of tears!
We use ICD-10 codes to document WHY medical procedures are performed. Bottom line – dietitians need to properly document the patient’s correct ICD-10 code(s) to get paid. This essentially represents the reason why the patient is seeking out your services. As dietitians, we need to put ICD-10 codes on both our insurance claims as well as on our Superbills. When using ICD-10 codes in electronic health records that code becomes a permanent part of the patient’s medical record. Therefore, selecting a medical diagnosis solely based on the patient’s report could expose the dietitian to possible claims of insurance fraud. But I know you guys are WAY too smart for that!
What diagnosis codes can dietitians use?
Once again just to repeat: IT IS NOT WITHIN THE SCOPE OF PRACTICE OF A DIETITIAN TO MAKE A MEDICAL DIAGNOSIS. Therefore, the main way for a dietitian to get the proper ICD-10 code for the visit is to request a referral from the patient’s physician for MNT.
If you are a member of The Academy of Nutrition and Dietetics you can find a list of commonly billed ICD codes under the Payment –> “Billing” tab.
Reimbursement Dietitian Tip: I might suggest if you commonly see (or are considering seeing!) a similar type of patient in your practice (e.g. eating disorders, renal patients, diabetic patients) that you include those diagnosis codes on your MD referral form. Therefore, when requesting a referral for MNT all the doctor needs to do is check the proper diagnosis, sign, date and provide their NPI number on the nutrition referral form.
Are there exceptions in which dietitians can determine the diagnosis?
Yes, Mama! Like with most things in life there are exceptions. The ONLY exception in which a dietitian can determine a diagnosis is in the case of BMI codes. It is within the scope of practice of a dietitian to calculate a patient’s BMI code. Depending on a patient’s particular insurance and policy, a BMI code can often be used with the preventative code Z71.3. This code is a billable ICD code used to specify a diagnosis of dietary counseling and surveillance. We use it in combination with a patient’s BMI code.
Here is a list of adult and pediatric ICD-10 codes for BMI.
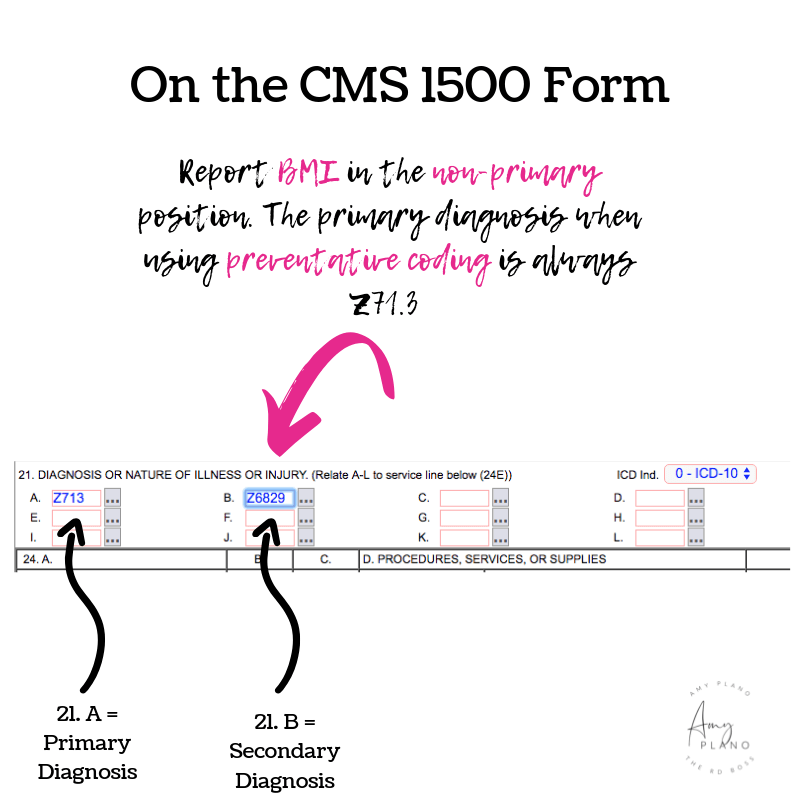
When billing, both the adult and pediatric BMIs are reported as a non-primary diagnosis (in position B, section 21 on the CMS 1500 Form). For adults, dietitians use ICD-10 codes Z68.1 – Z68.45. BMI adult codes are for use for persons 21 years and older. For pediatric patients (age 2-20 years old), dietitians can use ICD-10 codes Z68.51 – Z68.54.
Please note the BMI codes are not necessarily linear. Meaning, if an adult patient has a BMI of 44 you would use Z68.41 NOT Z68.44. Once you start billing insurance companies (which if you aren’t already – hopefully will be doing SOON!) I would suggest printing out a little ‘cheat sheet’ to keep handy with all the BMI codes. While most of them are self-evident, as you can see, some of them aren’t. If you bill with the wrong BMI code and hence, the wrong ICD 10, the insurance company will often deny the claim. Oh, the joys of being a private practice dietitian!
How does a dietitian request the diagnosis code?
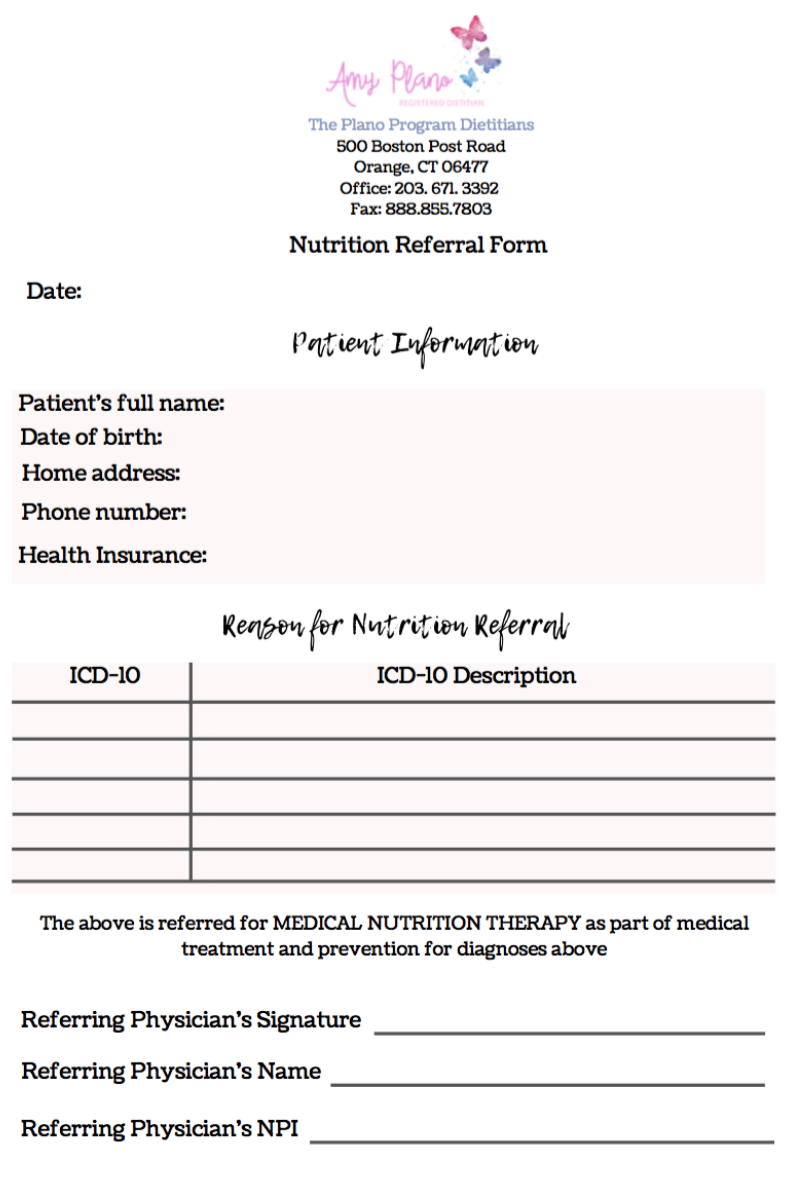
When at all possible, dietitians in private practice should obtain a formal nutrition referral from the patient’s physician or another qualified non-physician practitioner (e.g. nurse practitioner, physician’s assistant). The referral should be typed on your business’ letterhead and include a spot for the doctor to put the patient’s name, date of birth, home address, and phone number. It should also have a spot for the doctor to put the proper ICD-10 code and a brief description of the ICD-10. There should be a spot for the doctor to sign, date and document his/her NPI. The nutrition referral form can be faxed to the doctor.
Here is an example of the nutrition referral form I use in my practice The Plano Program:
I created the form in Canva and then used PDFescape to make it editable. This way I can just fax over the form and they can directly fill it out and fax it directly back. Easy-peasy! While I pay for the business version of Canva, there is a FREE version that is equally as fabulous. I highly recommend both FREE programs.
Need a physician referral form? The Reimbursement Dietitian has got you covered! Check out The Reimbursement Dietitian – Starter Pack complete with all the important forms you need to start the nutrition private practice of your dreams.
Conclusion
So, if you learned (or relearned) anything from this blog, I hope it was this – we as dietitians can’t determine a patient’s diagnosis. Even if we know for a fact a patient is obese, or they have an eating disorder or diabetes – we can’t, under any circumstances, diagnose the patient. What diagnosis codes can dietitians use to seek reimbursement? The list as you can see is long. Yay! But, we just need to make sure we get proper documentation noting the patient’s reason for their nutrition visit. This means we need to submit a proper MNT referral request to the patient’s medical doctor. The only exception is if the patient has preventative nutrition services covered on their insurance policy (which many patients do under the Affordable Care Act). Then we can use the ICD-10 code of Z71.3 plus the patient’s BMI code on the claim. Aside from that ladies – that’s all for now.
Need help getting credentialed, managing and growing your insurance-based practice? The Reimbursement Dietitian is the girl for the job. Click HERE to learn about how I help dietitians work with insurance in their practices.